The Who
105 registrants representing all areas of the Commonwealth met on March 15, 2023 in Norfolk, Virginia in a special pre-session of the Mid-Atlantic Telehealth Resource Center’s annual summit. Attendees included clinicians, state leaders, health system administrators, health plan leaders, public policy advocates, and industry representatives.
An additional 11 Virginians attended a virtual discussion on March 16.
The Purpose
The Virginia Telehealth Network, the Mid-Atlantic Telehealth Resource Center, and the Virginia Department of Health hosted this transformative discussion about shaping the future of telehealth in Virginia. The program featured:
- High-level policy discussions regarding changes needed at the federal, state, and local levels.
- Local innovations in telehealth that could present models for replication across the Commonwealth.
- Multi-sector dialogue regarding where Virginia wants telehealth to be in the next five years.
This “north star” conversation was intended to inform enhancements to the State Telehealth Plan. During the working session, attendees were invited to provide their input into the plan and help incorporate the latest research on telehealth implementation, best practices, and innovative models.
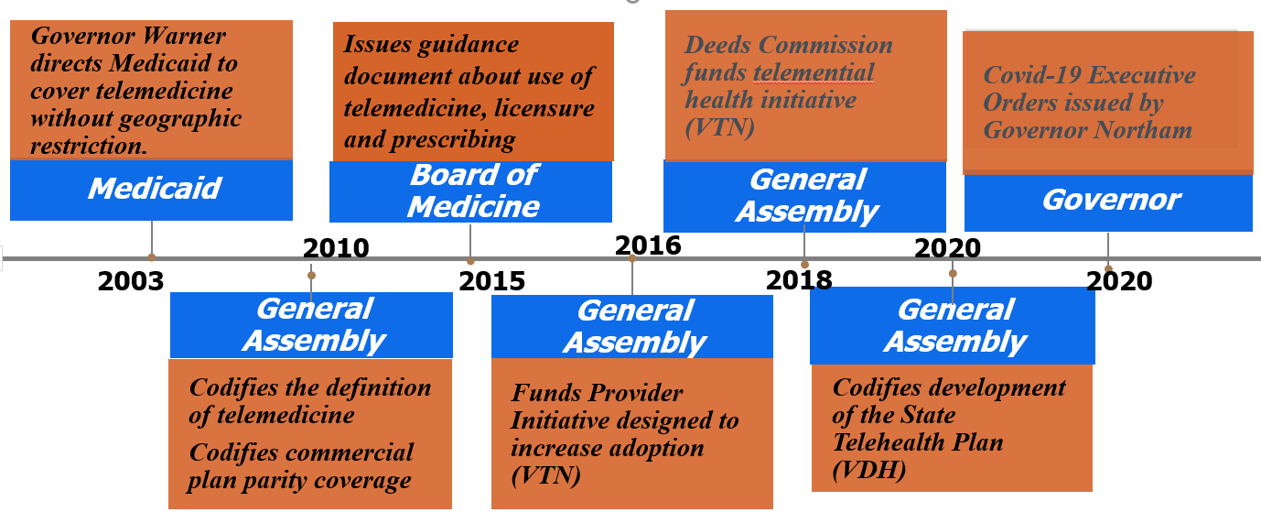
Virginia’s Timeline of Telehealth Successes
Virginia’s State Telehealth Plan
Virginia’s State Telehealth Plan was adopted by the Board of Health in 2021. To access the current plan, along with process and meeting information, visit https://www.vdh.virginia.gov/commissioner/board-of-health/state-telehealth-plan/.
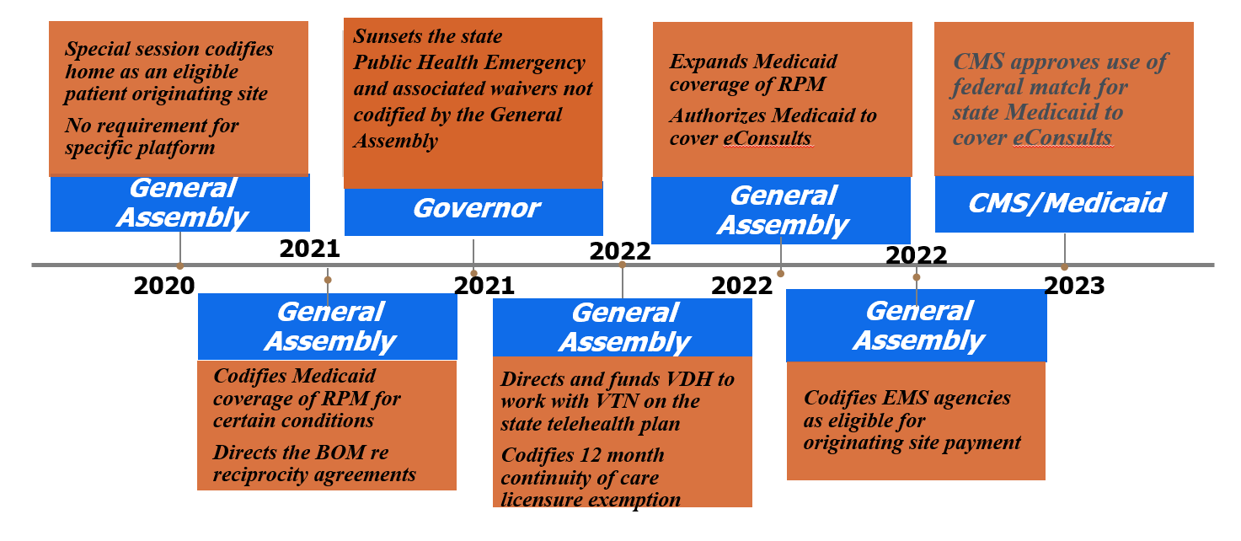
The Discussion Framework
Strengths: What successes and lessons-learned can we build on?
- Virginia is a national leader in telehealth policy and innovation
- Virginia legislators and government leaders have been champions for telehealth
- Medicaid expenditure data during the COVID-19 pandemic showed telehealth services are largely substitutive
- Telehealth waivers and subsequent legislative changes enabled a significant scaling of telehealth services
- Improved access to mental health care
- DMAS accessibility and responsiveness
- Community paramedicine innovations
- Cross-organization information and resource sharing
Opportunities: Where should we prioritize our efforts?
- Telehealth is a critical element of care re-design
- Alignment across payers; public policies must stay abreast with innovations in health care
- Criteria for use of telehealth intervention
- Reciprocity for when patients travel out of the area
- Reconsider BOM definition of practice of medicine with regards to established patients to deal with distinction between asynchronous with prescribing vs without
- Integrated care model: right sizing of virtual care is still a work in progress
- Creative problem solving for enhanced access:
- School-based telehealth offers enhanced access, less missed learning, and supports caregiver work-life balance
- Permanent telehealth space within clinics to help patients who cannot access technology from home
- FQHC servicing as distant site
- Technology: broadband access, health information exchange, identifying community-based collaborative care settings
- Advance conversations on alternative payment models, building upon lessons learned from fee-for-service
- Interstate compact for licensure
- Virginia continuing its role as a national leader in telehealth advocacy.
Aspirations: What are you most excited about from this information?
- Workforce development
- Opportunities to support providers experiencing burnout
- Opportunities to address provider shortages
- Leveraging telehealth and paraprofessionals
- What other services can be addressed through telehealth to improve access?
- Investments in digital health and value-based contracting
- Continued improvements gained via telehealth: improved no-show rates, improved access to psychiatric care, improved access to timely appointments
- Opportunities to integrate lessons learned in various use cases and care settings (e.g., primary care integration, teledentistry, correctional facilities)
- Quality is about reducing variability; how can virtual care enhance quality best?
Results: How will we know we made an impact?
- Improved access to care and reduction in barriers to receiving care:
- Enhanced technology access for low-income adults
- Reduction in transportation as a barrier to care
- Ensuring functionally equivalent access for Relay users in Virginia; inclusive of Video Relay (VRS), Captioned Telephones, TTY, Voice Carry Over (HCO) as well as Speech to Speech (STS) relay
- Trauma-informed practices
- Continued bipartisan support
- Less complexity in care delivery (e.g., simplifying billing and coding, reduction in administrative burden)
- Patient satisfaction, provider satisfaction
- Utilization, costs per visit, reduction in duplicative care, improved patient compliance
- Improved clinical outcomes:
- Earlier detection, better management of chronic illnesses
- Reduction in ED visits, reduction in unnecessary hospitalizations, reduction in readmissions
- Telehealth becoming a standard of practice as a mode of health care delivery
- Maximize the goals of telehealth and minimize fraud/waste/abuse and low quality services
- Telehealth will be standardized and on par with in-person care where appropriate
- Patients receiving the right care at the right time
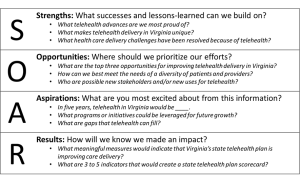
The following slides were sourced from a presentation on Quality and Telehealth led by Peter Fournier, Director, Product Development, National Committee for Quality Assurance (NCQA) during the VTN 2023 Summit.