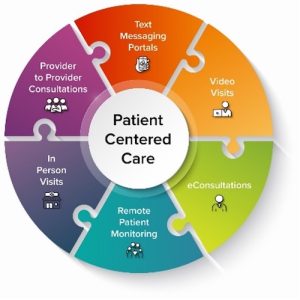
The swift growth of telehealth rapidly transformed health care delivery. Flexibilities during the Public Health Emergency enabled providers to adopt new ways in how telehealth technologies can be used, ranging from text messaging portals and eConsultations to video sessions with patients or other providers.
As providers and patients alike quickly adjusted to new models of virtual care, patient safety concerns became more defined. Below are considerations and best practices to foster a secure and effective telehealth environment.
- Standardized protocols: Determine what type of telehealth model works best for your patient population. Develop standardized protocols for telehealth appointments, covering issues such as patient identification, emergency procedures, and technology requirements.
- Privacy and confidentiality: Telehealth appointments often take place in patients’ homes, creating unique challenges for privacy. Encourage patients to choose a quiet and private location for virtual appointments. Advocate for the use of secure and encrypted platforms to protect sensitive information.
- Health equity: Not all patients have equal access to broadband or technology, which is especially true in underserved and rural areas of Virginia. Work with your patients to identify if telehealth is a suitable solution for them. Connect with local community resources that can get patients connected to necessary technology for telehealth sessions. Commonwealth Connection and Virginia Wifi Hotspot Locations are online tools that allow Virginians to find access to free broadband at a location near them.
- Emergency preparedness: In certain urgent situations, in-person care may be immediately needed. Educate patients on when to seek emergency care and provide clear instructions for accessing local emergency services. Set expectations regarding the limitations of telehealth in handling critical medical situations.
- Provide patient education: In addition to education for emergency situations, teach patients about the proper use of telehealth services and address any concerns they may have. Provide written materials or video tutorials to guide patients.
- Medication safety management. Conduct a thorough medication reconciliation to review the patient’s current medications, allergies, and potential drug interactions, and integrate multidisciplinary team members when needed. Provide clear instructions and education to patients and caregivers regarding medication dosage, administration, and potential side effects.
- Regular audits and assessments: Regular audits of telehealth systems can help to identify and address potential vulnerabilities. Seek feedback from both health care providers and patients to continually improve the telehealth experience.
- Continuous training for health care providers: Train health care professionals in telehealth best practices and encourage ongoing learning to stay updated on technological advancements and safety measures.
Additional Resources
- The Institute for Healthcare Improvement observes “Patient Safety Awareness Week” each March, providing educational resources and virtual events.
- Patient Safety 101: The Fundamentals, Patient Safety Network
- Interoperable Telehealth: Patient Safety Considerations, The Doctors Company Group
- Findings and Recommendations: Patient Safety and Program Integrity, National Committee for Quality Assurance (NCQA)