As part of Virginia Telehealth Network’s commitment to serving those who need it most, we kicked off our Equity & Telehealth initiative with an introductory webinar led by Dr. Sadiq Patel, NIMH Postdoctoral Research Fellow at Harvard Medical School within the Department of Health Care Policy.
During this session, Dr. Patel introduced to our members a high-level overview of how we should think about equity and telehealth in a post-pandemic world by examining the landscape both pre and during the pandemic. Here are a few highlights from the session.
Telemedicine in a pre-pandemic world
Before the widespread of COVID-19 in the United States, telehealth was largely focused on rural areas. But with that focus came several policy challenges and restrictions in its use including:
- Limited use to specific procedures, e.g., CPT codes.
- Reimbursements were not at parity to in-person visits.
- Telemedicine visits were not conducted in a patients’ home.
- The requirement that a patient-provider relationship be established in person.
- State licensure requirements limiting providers to only visit with patients within their licensed state to practice.
From 2010 through 2017, there was a spike in the use of telemedicine yet remained scarcely used. And those who did use it were primarily specialty or telemental health care providers.
The rise of telehealth during the pandemic
In March 2020, telemedicine policy temporarily changed, and restrictions previously mentioned were lifted as part of the declaration of emergency in Virginia. For example, Medicare expanded procedures that became reimbursable via telemedicine; telehealth now included both rural and urban areas; reimbursements became at parity with in-person visits; and telemedicine visits can now be conducted at home, etc.
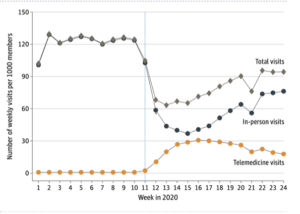 When these changes went into full effect, there was an explosion in the use of telemedicine, though not without some unease.
When these changes went into full effect, there was an explosion in the use of telemedicine, though not without some unease.
“A big concern during the pandemic, after many restrictions around telehealth were lifted, was in ensuring growth in telehealth due to COVID-19 did not exacerbate disparities in care,” Dr. Patel said.
When viewing the geographic distribution of where telemedicine visits were happening during the pandemic, Dr. Patel’s research takes a dive into distinguishing what drove the use in those areas as well as differentiating who was using it by looking at patients’ race, socioeconomic status, geographic variations etc.
Looking ahead
As the industry moves forward in a post-COVID world, will telehealth be a mechanism for underserved communities to have access to care or will individuals in affluent areas use it for convenience?
Dr. Patel emphasizes the urban and rural divide, among other disparities, that will require targeted policy to address items like access to broadband and digital technology, payment rate for telemedicine in rural areas, removal of all regulations for FQHCs and much more.
“We need to be thinking about the community members that will be left behind and no longer able to access telehealth; we need to look at the framework of telemedicine not as having a single policy but through the lens of its value; and more importantly, we need to look at the data around telemedicine during the pandemic,” Dr. Patel said.
VTN members, to access the full recording of the Equity in Telehealth Kickoff Webinar, click here.

